The Nursing Associate's Handbook of Clinical Skills
Здесь есть возможность читать онлайн «The Nursing Associate's Handbook of Clinical Skills» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:The Nursing Associate's Handbook of Clinical Skills
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
The Nursing Associate's Handbook of Clinical Skills: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «The Nursing Associate's Handbook of Clinical Skills»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
The Nursing Associate’s Handbook of Clinical Skills
The Nursing Associate’s Handbook of Clinical Skills
The Nursing Associate's Handbook of Clinical Skills — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «The Nursing Associate's Handbook of Clinical Skills», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
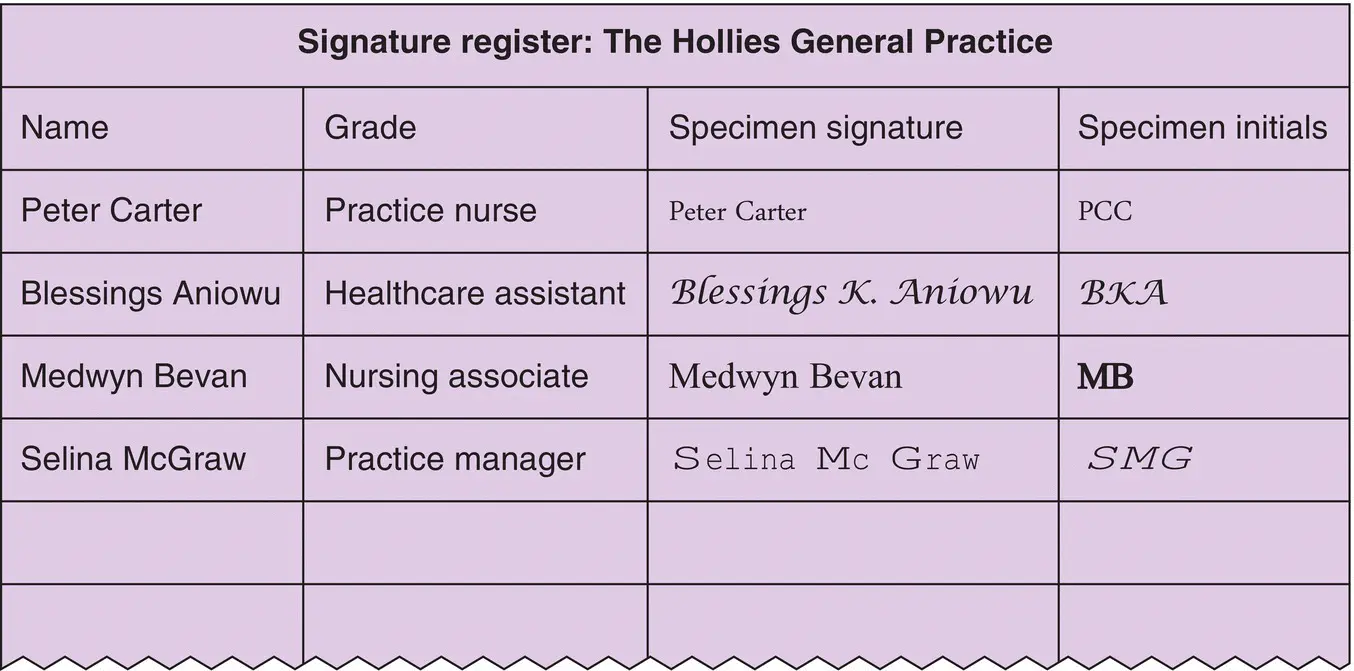
Figure 8.1 An example of a specimen register used in a general practice.
One of the final subsections within Section 10 requires the nursing associate to make sure that all records are clearly written, dated and timed, and that they do not include unnecessary abbreviations, jargon or speculation. As this subsection contains detailed guidance for record‐keeping, this will be now discussed in several sections. These requirements of the NMC Code are also echoed by the NMC proficiency standards (2018) that state that records are to be written accurately, clearly and legibly. Accuracy and clarity are quite inseparable. The nursing associates must also remember that there will be quality standards in their workplace that will govern how they are required to undertake documentation; they must not deviate from these standards.
Touch Point
Think about a record that you have written. Was this record both accurate and clear? How could this be improved?
Legible and Clearly Written
These are two terms used by the NMC which possibly have similar meaning, although clearly written could be interpreted as more than just legibility. To reiterate, the nursing associate must ensure that all records are made in such a way that they can be read by another healthcare and social care professional. Legibility is therefore very important to ensure that all records made communicate necessary information about the patient for whom the record has been made. As discussed previously, when looking at who has access to records, it was seen that a number of professionals, including the legal community, police as well as healthcare and social care professionals can also access records, and as such, content must not be ambiguous or difficult to read or decipher. Legibility requires that when a record is made by hand, black indelible ink is used, and pencil must not be used as this can be erased and rewritten at any time. Furthermore, many pencil leads fade with time; therefore, this does not make a permanent record. Often, local policy requires all record makers use black ink as this can be more permanent and photocopies and scans better than blue ink. If in doubt as to what a local policy is on record‐keeping, then using black ink is always a safe default position; you must seek advice if you are unsure. Legibility is also concerned with the alteration of a record in a clear way. A record that has been clearly written will also consider other issues such as language.
Language
The language used in records must be unambiguous in its meaning. This requires that it is factual and not open to interpretation in any way which could lead to confusion and ultimately could result in a patient not receiving the care they need or care that may cause them harm. If a patient, for example, has had their vital signs measured and recorded every 15 minutes, then this frequency must be recorded rather than a simple entry to state that the patient’s vital signs have been measured. The fact that the reader now knows that the vital signs have been recorded every 15 minutes conveys a message that the patient’s needs are such that they require close monitoring.
Yellow Flag
 When making an entry in a record or documenting care outcomes, the nursing associates must ensure that entry that they are making in the record is factually correct. Only record what you, as the nursing associate, see, hear or do. Using emotive statements can hinder the nursing associate and other readers of records from making objective decisions regarding the patients and their care.
When making an entry in a record or documenting care outcomes, the nursing associates must ensure that entry that they are making in the record is factually correct. Only record what you, as the nursing associate, see, hear or do. Using emotive statements can hinder the nursing associate and other readers of records from making objective decisions regarding the patients and their care.
Another example would be if a patient is incontinent of urine and faeces, the written record should be identifying this rather than simply stating that the patient has been incontinent as this again does not fully and accurately convey or report on the needs of that patient. This would also have implications for future reviews to be completed; they may not be accurate as the information about the type of incontinence is not available to the next person undertaking a review. The subsequent reviews are also recorded, and as such, the principles of accuracy and clarity will also apply.
Red Flag
 When the nursing associate fails to document care provision in the correct manner, this can result in serious harm to a patient’s health and well‐being. These failures are attributable to human errors. Harm can occur when there is a wrong or delayed response to care, and this can be a result of failure to capture documented signs and symptoms and laboratory tests and failure to undertake, document and report care findings. Poor documentation, failure to read and understand a patient’s nursing and medical record, can put a patient at serious risk of harm.
When the nursing associate fails to document care provision in the correct manner, this can result in serious harm to a patient’s health and well‐being. These failures are attributable to human errors. Harm can occur when there is a wrong or delayed response to care, and this can be a result of failure to capture documented signs and symptoms and laboratory tests and failure to undertake, document and report care findings. Poor documentation, failure to read and understand a patient’s nursing and medical record, can put a patient at serious risk of harm.
Reducing the risk of patient harm during care delivery (and this includes documentation and record‐keeping) must be at the forefront of policy and practice, and the nursing associates have to ensure that all they do are done in the best interest of those they have the privilege to care for.
Jargon and Abbreviations
Language that is used in record‐keeping must also be jargon free. It is worth remembering that the language used in the record could be interpreted or misinterpreted by any of the previously mentioned groups, including families, patients, allied health professionals and external agencies such as the police. There are abbreviations that are commonly used in all walks of life such as National Health Service (NHS) which most people would know refers to the NHS; however, there are many times when jargon or abbreviations should not be used, for example, MI which could stand for myocardial infarction but could equally stand for motivational interview or DOD which could mean date of discharge or date of death.
This does not mean that medical terminology and abbreviations should not be used such as cerebrovascular accident (CVA) as opposed to writing stroke (note the convention of writing the term in full and then abbreviating the term afterwards. This gives clarity as to abbreviations and their meaning later in the record.) In this instance, it is the lay term stroke that has several meanings, whereas CVA is quite explicit.
Due to instances where a word used in a record has had different connotations and the appropriate or required action has subsequently not been forthcoming, the requirement for records to be made clear by being jargon free is apparent. Linked to this section, there has to be a consideration of spelling.
Spelling
Many computer programmes used for record‐keeping contain spell checkers, although these should not be relied upon as when words are not spelt correctly but the misspelled word is still a word, the spell checker would overlook this. For example, if the word ‘loose’ was mistyped as ‘lose’, this would have a different meaning, but as it may be a proper word, the mistake would be undetected by the computer. This highlights the importance of proofreading the entries, as other healthcare and social care professionals reading this record would assume that the patient had lost their bowels completely rather than having diarrhoea which is the intended message.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «The Nursing Associate's Handbook of Clinical Skills»
Представляем Вашему вниманию похожие книги на «The Nursing Associate's Handbook of Clinical Skills» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «The Nursing Associate's Handbook of Clinical Skills» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.