TABLE 3-1 Characteristics of the groups described by Löe et al 66in 1986

NA, not available.
MODELS OF DISEASE PROGRESSION
The patterns of disease progression have been extensively studied, aiming at evaluating how loss of attachment occurs over time. In 1982, Goodson et al 68described the progression of attachment level in 22 untreated patients performing measurements every month for 1 year. Results from this investigation demonstrated that the majority of the sites experienced no significant changes (82.8%), followed by 11.5% of the sites that became significantly shallower and 5.7% of sites that became significantly deeper. Within the group that suffered increase in probing depths, approximately half experienced progressive deepening and the other half presented with periods of exacerbation and spontaneous remission/recovery. 68In 1984, Socransky et al 69reviewed the available evidence and described three models of disease progression: continuous, random burst, and asynchronous multiple burst. 68In 1991, Jeffcoat and Reddy 70revisited this topic following patients with periodontitis for 6 months. In this investigation, three models were described as (1) linear or continuous (76% of sites), (2) burst (12% of sites), and (3) exacerbations and remission (12% of sites). 70
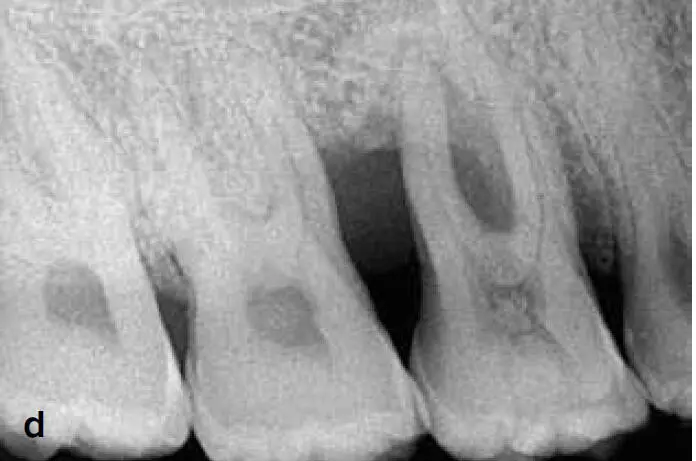
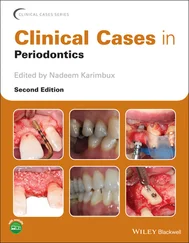
The term aggressive periodontitis has been through many modifications since 1923 when Gottlieb defined it as “diffuse alveolar atrophy.” 71Over the course of the 20th century, this inflammatory disease often changed in terminology, being referred to as periodontosis , juvenile periodontitis , and early-onset periodontitis , among others. Later, in 1999, the American Academy of Periodontology proposed the term aggressive periodontitis to refer to the highly destructive forms of periodontitis. 72This rapidly progressing type of periodontal disease has been studied for decades as a separate entity from chronic periodontitis due to its aggressive nature, familial tendencies, the location of the lesions, and the relative low or inconsistent levels of biofilm (and secondary etiologic factors) compared with the severity of periodontal tissue destruction 73,74(Fig 3-4). Other features recognized by the 1999 consensus report included patients that are otherwise healthy, rapid attachment loss and bone destruction that may be self-arresting, and phagocyte abnormalities. 7 3



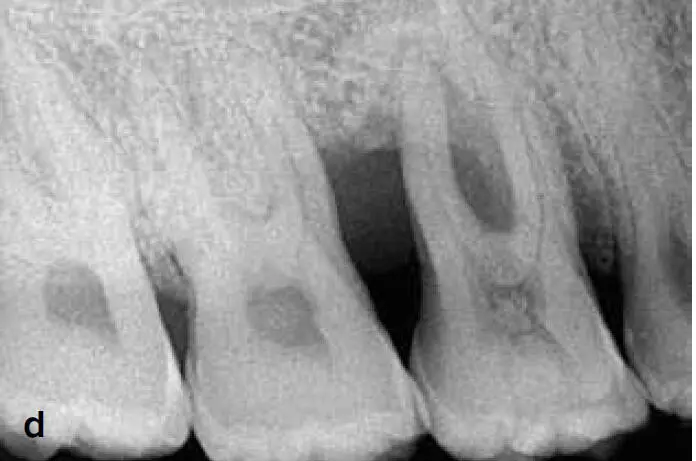


Fig 3-4 (a to f) Periodontitis (formerly referred to as aggressive periodontitis ).
Nevertheless, chronic and aggressive periodontitis share many similarities, and the latest classification from the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions refuted the presence of enough evidence to support the distinction between aggressive and chronic periodontitis as two separate diseases. This recent report emphasized the phenotypic differences between both entities, and more specifically, between chronic and localized aggressive periodontitis (including age of onset, location of initial lesions, and rate of progression). However, it also reiterated that both represent inflammatory diseases responding to biofilm accumulation, and it is premature to describe pathophysiologic differences until further data in larger and more controlled studies is available. In addition, both chronic and localized aggressive periodontitis have a common end result. 62Hence, it was concluded that while there are significant variations with regard to clinical presentations, the currently available evidence does not support the distinction between chronic and aggressive periodontitis as two separate diseases. 1
Periodontitis as a Manifestation of Systemic Diseases
Several systemic diseases and conditions can affect the periodontium and cause its destruction. Most of these disorders or conditions are secondary to innate mechanisms, although some are acquired through lifestyles or environmental factors. The periodontal effects of these systemic diseases and conditions are mainly through their influence on the immune and inflammatory responses. In addition, these can affect the periodontium by either influencing the course of periodontitis or by affecting the supporting tissues independently of plaque-induced inflammation. 75Albandar et al 75classified those diseases and conditions into three main categories. The first includes systemic disorders with a major impact on the loss of periodontal tissue by influencing periodontal inflammation. These disorders include genetic disorders (eg, Down syndrome), acquired immunodeficiency diseases (eg, HIV infection), and inflammatory diseases (eg, arthritis). The second category describes systemic disorders that influence the pathogenesis of periodontal diseases contributing to periodontal tissue loss (eg, smoking, depression). Last, the third category describes disorders that can cause destruction of the periodontal attachment independent of plaque-induced periodontitis (eg, neoplasms). 75
Most of these conditions are determined by the genotype of the host, and they may be modified by environmental and behavioral factors. In addition, periodontitis and certain systemic disorders may share similar genetic and/or environmental risk factors. Consequently, loss of periodontal attachment is a common manifestation of several systemic disorders, which could have an important therapeutic and diagnostic value.
Necrotizing Periodontal Diseases
Necrotizing periodontal diseases belong to a group of acute lesions occurring in the periodontium and can be divided into necrotizing gingivitis (formerly referred to as necrotizing ulcerative gingiviti s) and necrotizing periodontitis (formerly referred to as necrotizing ulcerative periodontitis). 76Currently available evidence suggests that given the similar etiology, clinical features, and treatment, these entities may represent different stages of the same disease and may even progress to more severe forms such as necrotizing stomatitis and noma. 76
Necrotizing periodontal diseases are associated with impairment in the host immune response and typically present with three clinical features: papilla necrosis, pain, and bleeding. Other signs and symptoms may include halitosis, pseudomembranes, regional lymphadenopathy, fever, sialorrhea, and rapid bone loss in cases of necrotizing periodontitis. Necrotizing stomatitis is a more severe inflammatory condition that courses with soft tissue necrosis beyond the gingiva, osteitis, and bone sequestrum. 1
Similar to other forms of periodontitis, the etiology of necrotizing periodontal diseases is a bacterial infection; however, several other predisposing factors and immune-related conditions play a role in the pathogenesis. 76
Читать дальше