A recurring theme of this book is the need in healthcare for greater kindness. Not kindness as simply an emotional feeling – important though this is – but intelligent kindness, the kindness that motivates us to be cooperative rather than competitive with one another; to feel connected, thoughtful and with a sense of kinship towards other people. This connectedness starts with thoughtfulness towards ourselves, and learning about the impact on our physiology and our cognitive performance of the stressful environments in which we are all working. The potential gains are substantial. First, there is our own well‐being, and a recovery of that ‘joy of practice’ which first alerted us to the attraction and fulfilment of working in healthcare. Secondly, greater safety and well‐being of staff means improved safety for patients and a reduction in the medical error related to staff burnout. There is a particular responsibility on healthcare regulators, leaders and providers to develop the intelligent kindness towards healthcare staff which has too often been absent, so that staff and their patients remain safe.
We are grateful for the contribution of our authors, all of whom committed to this project before the outset of the Covid‐19 pandemic, an event which has bought into much sharper focus so many of the themes we set out to explore in this book. They have shown resilience in completing their chapters in such a timely way despite the challenging circumstances. We work in Canada and the UK, and so this book inevitably reflects perspectives on resilience in our particular countries. However, from our professional conversations, we believe the themes we have explored reflect concerns in many countries and health systems worldwide.
We hope the individual reader will find this book of interest. With our emerging understanding of resilience and its importance to patient care, training programmes are increasingly considering how to incorporate resilience into healthcare education. We hope our work will be helpful to them as well.
Anna Frain
Sue Murphy
John Frain
February 2021
CHAPTER 1 Why resilience? Why now?
Anna Frain1, Sue Murphy2, and John Frain3
1University of Nottingham, Graduate Entry Medical School, Derby Speciality Training Programme for General Practice, Nottingham, UK
2Faculty of Medicine, Department of Physical Therapy, University of British Columbia, Vancouver Campus, Canada
3Division of Medical Sciences and Graduate Entry Medicine, University of Nottingham, UK
Those entering healthcare professions are motivated by the potential ‘joy of practice’.
Healthcare practitioners are being harmed by the impact of the systems in which they work.
Burnout is an occupational hazard for all healthcare workers and increases the risks of both major and minor errors in caring for patients.
Equality and inclusion in healthcare are not only morally right but enables all to fulfil their potential to improve patient outcomes and maintain practitioner well‐being.
The Covid‐19 pandemic has brought into sharper focus the impact and current challenges of the working environment upon healthcare workers.
Organisations have a duty of care to protect patient safety by supporting healthcare workers with intelligent kindness.
Healthcare workers are human beings trying to help other human beings. This invariably leads to a discussion of human frailty and shortcomings. Yet, the skills and abilities of practitioners are awesome, and we often have an insufficient sense of awe regarding them – to listen and to understand the effects of suffering on patients, to use our senses to examine and to diagnose, to provide comfort and support, to restore to health, to witness both the greatest joys in patients’ lives as well as their darkest moments. Undoubtedly, this work requires the full use of our talents and is rewarded by the joy of practice.
Alongside this, advances in treatments across the multidisciplinary spectrum of healthcare in the past century enables us to do more and achieve more for patients and to genuinely feel we are making a difference to peoples’ lives. Those entering healthcare training should be confident they are entering an occupation at the cutting edge of human endeavour and characterised by the sense of the well‐being and resilience of those working in it.
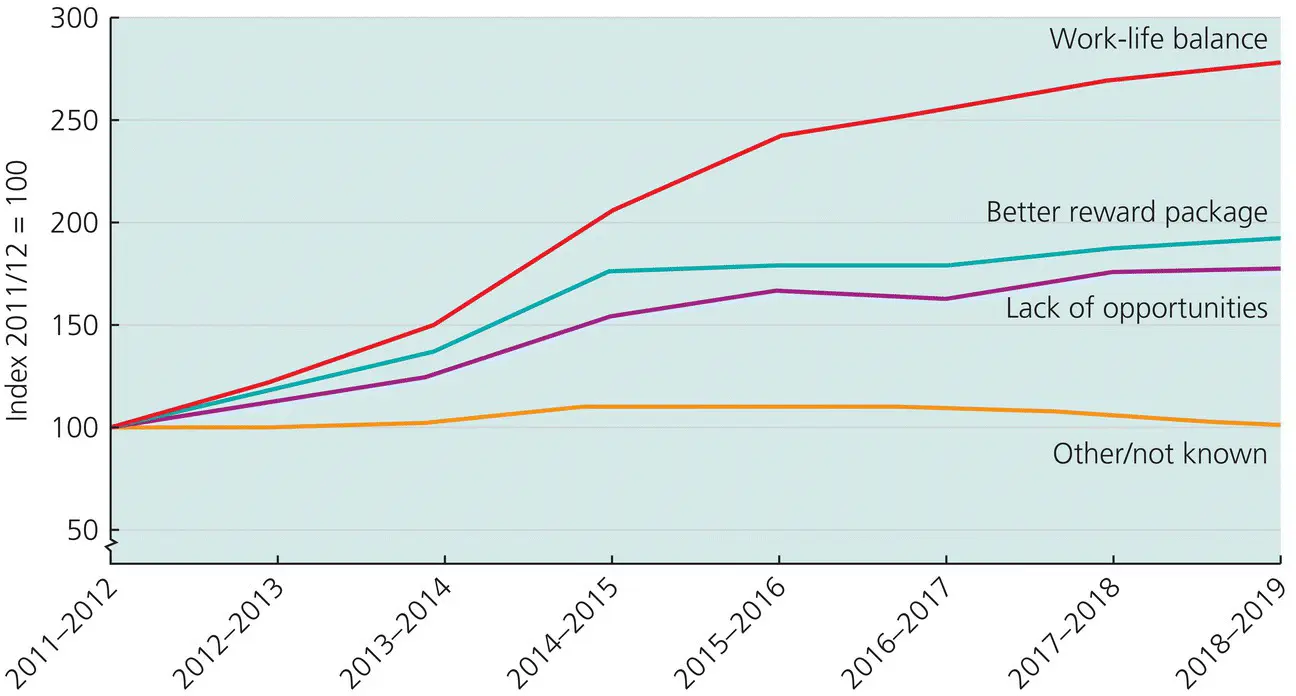
Yet, the reality for many practitioners is very different. Confronted by the uncertainties and ambiguities of practice as well as the stresses of the healthcare environment, new entrants to the professions show increased reluctance to undertake specialty training, deciding to take career breaks or leave the profession completely ( Figure 1.1). This established problem is so significant and widespread that it must be considered to genuinely threaten the future sustainability of modern healthcare. Resilience implies an ability to ‘bounce back’, to regain our well‐being after a distorting experience. The data suggests we are not bouncing back as well as perhaps we once did. This is impacting patient care and providing immeasurable harm to healthcare providers.
For UK healthcare professions, the past decade is bookended by two events. First, a private citizen’s Freedom of Information request in 2012 led to the publication of an internal review by the General Medical Council (GMC) which revealed that, during the 2005–2013 period, 28 doctors had committed suicide whilst undergoing the GMC’s fitness‐to‐practice (FTP) investigations (Horsfall, 2014). Casey and Choong argued that these deaths were preventable and the GMC has a duty of care towards doctors under investigation (Casey and Choong, 2016) ( Box 1.1).
Practitioner suicide and distress is not unique to the UK, nor is it confined to doctors (Hofmann, 2018). Nonetheless, these healthcare professionals likely entered training with the same aspirations and hopes as their peers. In their deaths, they left behind people who loved and needed them. A healthcare culture which seemingly leaves people viewing suicide as their only alternative should concern us all – as John Dunne said, ‘Any man's death diminishes me, because I am involved in Mankind’.
Second, the initial phase in the UK of the Covid‐19 pandemic was characterised by shortages of personal protective equipment (PPE), with the result that staff felt they were being required either to place themselves at risk without adequate protection, or to decline to care for patients and risk disciplinary action. This impression of a lack of concern for healthcare staff reached its apotheosis when a prominent UK politician suggested that shortages of PPE were occurring due to wasteful usage by healthcare staff (see Chapter 6). Subsequently, reports emerged of higher‐risk staff feeling unable to request the PPE to which they were entitled .
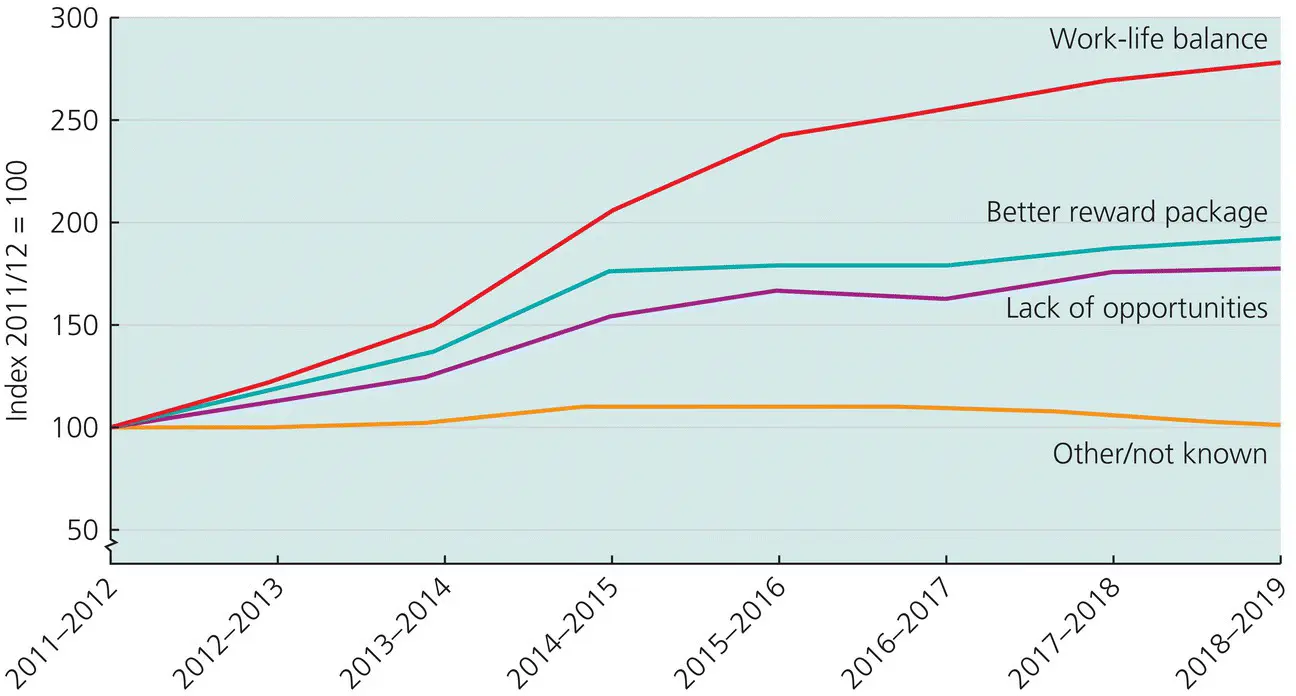
Figure 1.1 Change in reason for leaving given by staff (for voluntary resignations), 2011–2012 to 2018–2019 (Index at 2011/2012 = 100).
Source: The Health Foundation (2019). © 2019, The Health Foundation.
On a more mundane level, healthcare staff report day‐to‐day shortages in their work in terms of access to food, rest breaks and adequate on‐call facilities, such that these provisions are not in step with employment law (GMC, 2019). Even a cursory look at Maslow’s triangle ( Chapter 3) suggests that meeting a practitioner’s basic psychological and physical needs is required to safeguard and provide support for the high‐level problem‐solving necessary in clinical decision‐making; it is unlikely that depriving people of food, drink and adequate rest improves patient safety. When we consider clinical resilience, it is important that we do not impose on practitioners yet another burden of fearing failure. Rather, it is about enabling clinicians to optimise their cognitive performance, be the best they can be and recover the joy of practice. In this, organisations have a particular responsibility ( Chapter 8). With resilience, our recurring theme is kindness. Kind health systems and organisations will more greatly facilitate the potential of their teams and the safety of patients.
Читать дальше