Ridley's The Vulva
Здесь есть возможность читать онлайн «Ridley's The Vulva» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Ridley's The Vulva
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
Ridley's The Vulva: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Ridley's The Vulva»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Ridley’s The Vulva
Ridley’s The Vulva
Ridley's The Vulva — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Ridley's The Vulva», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
7 18 Vaccaro, CM. The use of magnetic resonance imaging for studying female sexual function: A review. Clin Anat. 2015 Apr; 28(3): 324–330.
8 21 Micheletti, L., Bogliatto, F. and Lynch, P.J. Vulvoscopy: Review of a diagnostic approach requiring clarification. J Reprod Med. 2008 Mar; 53(3): 179–182.
8 Topical and Non‐Surgical Treatments
Fiona M. Lewis
CHAPTER MENU
Topical treatments
General vulval hygiene
Types of preparation Emollients Barriers Topical steroids Adverse effects Calcineurin inhibitors Adverse effects Imiquimod Adverse effects Potassium permanganate Lubricants
Non-surgical treatmentsPhototherapy and photochemotherapy Photodynamic therapy (PDT) Adverse effects
Resources
References
Topical treatments
Topical treatment used for vulval disease may need to be modified from that used to treat the same disease at another site. For example, strong tar preparations or Vitamin D analogues used to treat psoriasis on the scalp or limbs may be very irritant in the anogenital area. This chapter looks at the general principles of topical and non‐surgical treatments and their potential adverse effects.
General vulval hygiene
It is important to ask about hygiene practices as these can vary with cultural influences and personal preference [ 1]. Many women feel the need to clean the vulva several times a day as they are often worried that a lack of hygiene on their part may have contributed to their vulval symptoms. Transepidermal water loss from the thinner vulval skin is greater than that from the forearm and is therefore more susceptible to the irritant effects of any application.
Simple washing once daily is required to wash away secretions and sweat. Soap removes the natural lipids produced by epithelial cells that have an important role in the integrity of the skin barrier, and so using an emollient as a soap substitute is encouraged. A bland ointment‐based emollient such as emulsifying ointment is preferred because of the low allergenic potential with this substance. Creams and lotions often contain preservatives which can be irritant and may sting if the skin is fissured. Several over‐the‐counter products can affect L. crispatus counts, which will alter the normal microbiome and increase the likelihood of inflammation [2]. The use of these products is widespread, with over 50% of post‐menopausal women questioned reporting use of at least one product [3].
Types of preparation
In any topical preparation, the active ingredient is mixed with a chosen vehicle to allow its delivery into the stratum corneum and to maintain the stability of the drug. Increased penetration of a drug can occur if the skin is inflamed or applied in occluded sites.
The majority of topical preparations used for vulval disorders are either ointments or creams. Gels and lotions often sting and are not widely used, but may be helpful in the hair‐bearing mons pubis area. Ointments are water‐in‐oil emulsions and form an impermeable layer over the skin that prevents evaporation of water ( Figure 8.1a). Due to their occlusive and hydrating effects, they can increase penetration of the drug. They are stable compounds which rarely require the addition of preservatives and hence have a much lower risk of inducing a contact allergy.
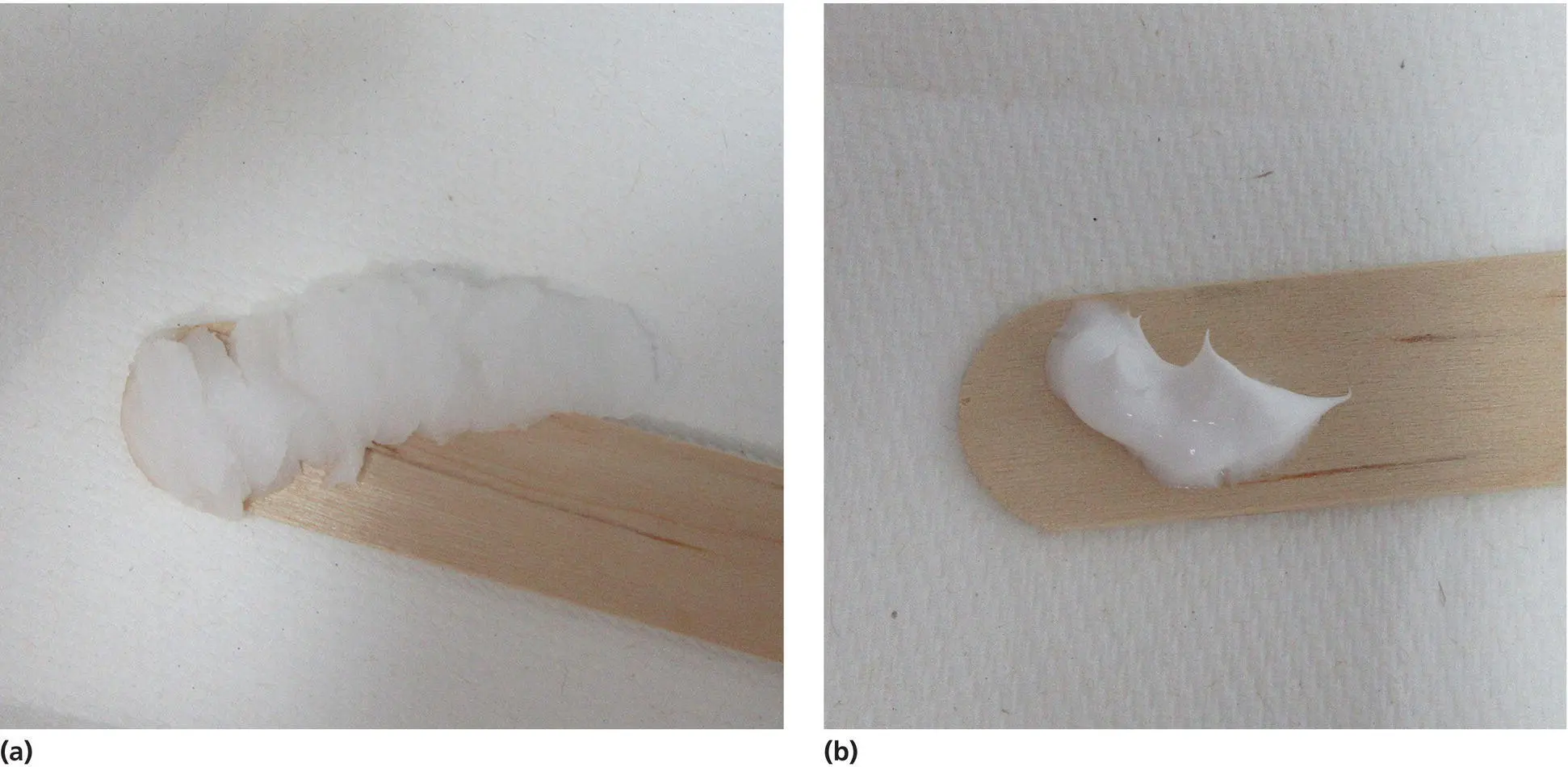
Figure 8.1 (a) Ointments are thicker and greasy to apply, but better to use in the anogenital area. (b) Creams are thinner and apply easily, but contain more excipients.
Creams contain oil and water. They are less greasy than ointments and spread more easily ( Figure 8.1b), but their high water content requires the addition of preservatives to prevent contamination by bacteria and fungi, and to prolong shelf life. It is important to remember that preservatives, stabilisers, and other additives are all components of topical treatment, and if the cutaneous problem flares after application of the preparation, it may be due to an allergic contact dermatitis to one of these agents and should be investigated as such (see Chapter 22).
Emollients
Emollients are an important part of the management of any vulval disease. In addition to their use as soap substitutes, emollients can also be applied directly if the skin is dry. They provide moisture, lubrication, and provide a mild barrier function. Ointments are always preferable to creams.
Barriers
Barrier preparations, for example, zinc and castor oil cream or petroleum jelly, can be useful to protect the skin from the irritant effects of urine. Patients with erosive dermatoses, such as lichen planus, can also benefit from these.
Topical steroids
Topical steroids were first used in the 1950s and revolutionised the treatment of many dermatoses, although the mechanism of their anti‐inflammatory action is not fully understood. Since the initial introduction of topical hydrocortisone, many different compounds have been formulated, and they are ranked in order of potency by their ability to produce vasoconstriction on the skin [4]. In the United Kingdom, there are four classes of topical steroid, whereas in the United States there are seven categories (see Tables 8.1and 8.2). The classification of some steroids differs in each system, which may lead to confusion.
A combination preparation of a topical steroid with an antibacterial or anticandidal agent can be useful if there is secondary infection, but sometimes the antimicrobial agent can be the cause of a contact allergy. It is helpful to become familiar with at least one preparation from each category, and to tailor the strength and vehicle to the clinical situation. Ointment formulations are always preferable.
If used correctly, topical steroids are safe on the vulva [5, 6]. Patients are often anxious about the potential side effects and therefore do not use them adequately to obtain the optimum results. Their worries can be further reinforced not only by family and friends but also by healthcare professionals. Many of the product information leaflets included in the packaging state that they should not be used on the genitalia, and a thorough explanation on the safe use of topical steroids for vulval disease needs to be given to the patient. Topical steroids are safe to use in pregnancy, and a systematic review shows no link of exposure to topical steroids and pregnancy outcome [ 7]. There was a possible link of low birth weight with the use of large quantities of topical steroids, but this would not be relevant for the small amounts used to treat the vulva.
Table 8.1 UK classification of topical steroids.
| Class | Potency | Examples |
|---|---|---|
| I | Mild | 1% hydrocortisone |
| II | Moderate | Clobetasol butyrate 0.05% Fludroxycortide |
| III | Potent | Betametasone valerate 0.1% Betamethasone dipropionate 0.05% Mometasone furoate 0.1% |
| IV | Superpotent | Clobetasol propionate 0.05% Diflucortolone valerate 0.3% |
Table 8.2 US classification of topical steroids.
| Class | Potency | Examples |
|---|---|---|
| I | Superpotent | Clobetasol propionate 0.05% Betamethasone dipropionate 0.05% |
| II | Potent | Mometasone furoate 0.1% |
| III | Upper mid‐strength | Betamethasone valerate 0.1% |
| IV | Mid‐strength | Fluocinolone acetonide 0.03% |
| V | Lower mid‐strength | Fluticasone propionate |
| VI | Mild | Fluocinolone acetonide 0.01% |
| VII | Least potent | 1% hydrocortisone |
The vulva is an area that is naturally occluded and therefore the penetration of the steroid is enhanced. It has been shown that there is a ‘reservoir effect’ in flexural areas in which the steroid can stay in the stratum corneum for up to two weeks. The topical steroid therefore needs to be applied only once daily [8]. When deciding about the correct amount to prescribe, a useful measure is the fingertip unit [9]. This is the amount squeezed from a standard tube that covers the distance between the distal interphalangeal joint and the tip of the index finger and equates to approximately 0.5 g ( Figure 8.2). About half of this, or a pea‐sized amount, is adequate for one application to the vulva. In general, tapering regimens are used so that the frequency of application is reduced over time. This helps to prevent tachyphylaxis, where there is loss of effect with continuous treatment.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Ridley's The Vulva»
Представляем Вашему вниманию похожие книги на «Ridley's The Vulva» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Ridley's The Vulva» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.