Ridley's The Vulva
Здесь есть возможность читать онлайн «Ridley's The Vulva» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Ridley's The Vulva
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
Ridley's The Vulva: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Ridley's The Vulva»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Ridley’s The Vulva
Ridley’s The Vulva
Ridley's The Vulva — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Ridley's The Vulva», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
2 The skin should be stretched so that it is held taut, and the punch biopsy inserted and gently rotated with firm pressure. The sample will elevate and can then be removed at the base with sharp scissors or scalpel. It should not be crushed as it is removed. A small core of tissue is then obtained. The cervical biopsy forceps should not be used for vulval biopsies as they crush the tissue and do not provide adequate samples ( Figure 7.2). Diathermy and other techniques can be used for haemostasis, but not to remove the specimen as the heat artefact makes histological interpretation difficult.
3 The biopsy site can be sutured with an absorbable thin suture (4/0 or 5/0). For shave biopsies, haemostasis can be achieved with the application of silver nitrate.
4 Adhesive dressings are not helpful; a folded piece of soft gauze is adequate, which can be held in place with underwear.
Post‐biopsy instructions
Most biopsies heal well within 5–7 days, and if sutured, the sutures usually absorb in 10 days. For small punch biopsies, analgesia is rarely required, but if needed paracetamol should be used to avoid the increased bleeding tendency of aspirin. Simple instructions given to the patient and backed up with written information should include the following:
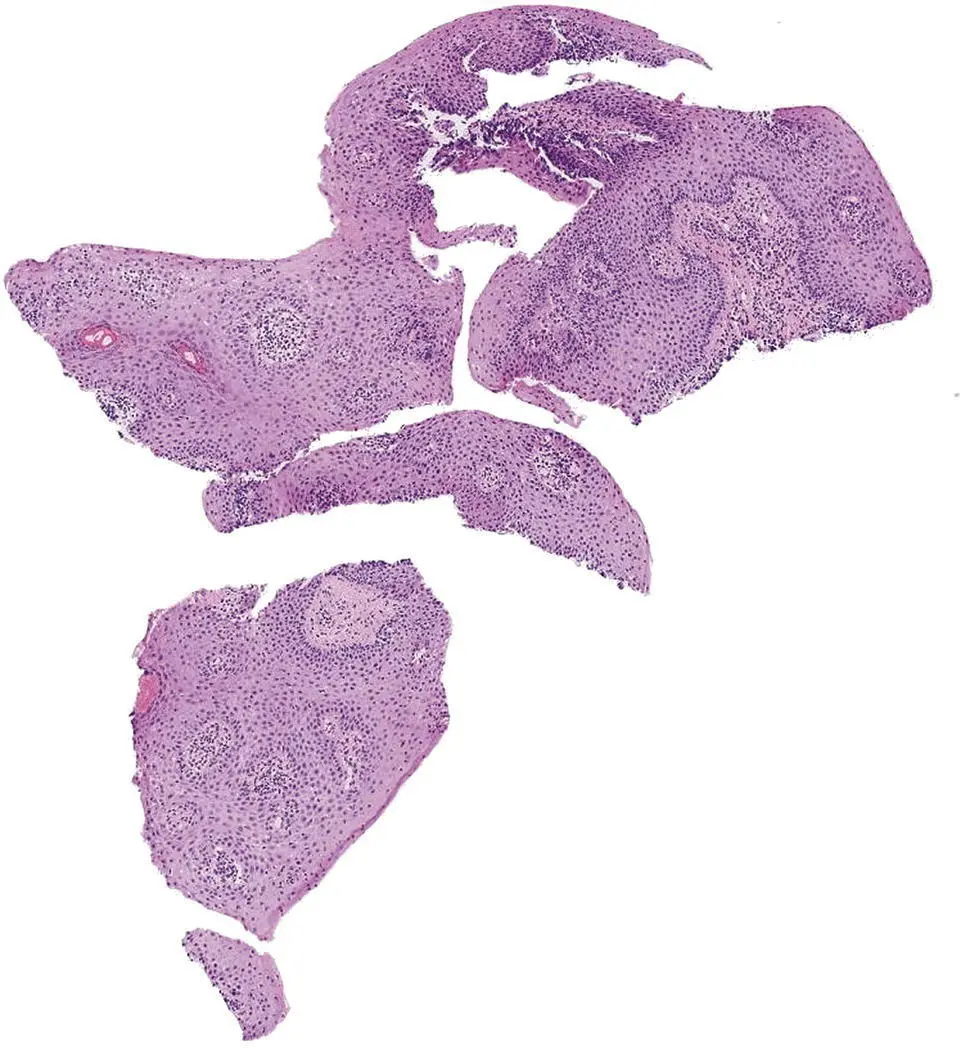
Figure 7.2 Example of poor biopsy technique resulting in a crushed specimen, which makes accurate interpretation impossible.
Avoid soaking the area in the bath for 48 hours, but showering is fine. The area should be cleaned daily.
Apply yellow soft paraffin to the area as a barrier before urinating to reduce any discomfort.
Avoid heavy exercise, swimming, or sexual intercourse until the area has healed.
If the area bleeds – apply firm pressure.
Signs of infection include erythema, pain, swelling, discharge, or fever, and then medical advice should be sought.
Samples
The biopsy specimen is immediately put into 10% formalin. If there are multiple biopsies, these must be put into separate pots and labelled correctly. Samples for direct immunofluorescence should be placed in Michel’s medium, which is a useful transport medium with the specimen being stable for 28 days [7]. Direct immunofluorescence (DIF) is used in the investigation of immunobullous disease and detects auto‐antibody/antigen complexes and uses fluorescent labelled antibodies to bind directly to the target antigen in the skin. There are specific immunoglobulins and binding patterns in different immunobullous disease (see Chapter 26).
Specimens for electron microscopy are put into liquid nitrogen or glutaraldehyde.
Documentation
The patient details on the sample pot must correspond to those on the request form. The procedure and instructions given to the patient should be documented. Most departments now use the WHO surgical checklist for this.
What do you need to tell the pathologist?
Clear clinical details must be given to the pathologist, which should include clinical features and the differential diagnosis. It is most helpful to supply them with a clinical photograph or diagram detailing the site of the biopsy. They also need to know whether topical treatment has been used and whether EMLA® was applied before the biopsy. As most vulval disease is dermatological, expert dermatopathological review is helpful. A multidisciplinary approach with clinicopathological correlation should be routine practice.
Cytology
The use of cytological techniques in the diagnosis of vulval disorders is limited, with conflicting results reported in studies. Poor correlation of vulval Pap smear cytology with subsequent histological analysis of neoplasia has been reported [8], but the specificity and sensitivity may be increased with the use of a scalpel technique [9]. Vulval brush cytology may be useful as a triage technique for deciding which patients may require a biopsy for clinically suspicious lesions [10]. Histological examination of a tissue sample should always be regarded as the gold standard.
However, for a rapid diagnosis of herpes simplex infection, a Tzanck smear is helpful.
Microbiological investigation
Swabs
Swabs can easily be taken for bacterial and yeast culture. A different swab put into transport medium is needed for viral cultures. If a sexually transmitted infection is suspected, the patient should be referred to a genitourinary medicine clinic for full investigation, screening, and contact tracing.
Scrapings
If a fungal infection is suspected, skin scrapings will be needed. These can be taken with a broad ‘banana’ blade and the edge of a scaly lesion gently scraped. The scrapings are collected on to a dark paper package for transport to the laboratory. If there is extensive involvement of a hair‐bearing area or a deep fungal infection is suspected, culture of a biopsy taken into a dry pot is helpful.
Serology
Serology may be needed to confirm some infectious diseases (see Chapter 9– 20).
Wet mount microscopy
This is a simple technique used in the investigation of vaginal discharge. A sample taken and placed in normal saline or 10–20% potassium hydroxide gives rapid results and is particularly helpful in assessing lactobacilli [ 11].
Wood’s lamp examination
The Wood’s lamp is a device that emits ultraviolet rays but includes a filter of barium silicate to exclude visible light. It is easy to use but is much less reliable in darker skin types because of the high levels of melanin present. It requires a completely dark room, and it is important to remember that false positive results can be achieved with scales, soap, residual topical treatment, or dressings. It can be helpful in diagnosis for a variety of dermatological diseases and infections [ 12]. It is also used to delineate the margins of lesions to be treated with photodynamic therapy after the 5‐ALA cream is applied (see Chapter 8). The conditions that are relevant to the vulva and the results expected are shown in Table 7.1.
Patch testing
Patch testing is a measure of delayed type (type IV) hypersensitivity and is used to investigate a suspected allergic contact dermatitis (see Chapter 22). It is of no value in the investigation of urticarial (type I) reactions.
Small amounts of allergens in suitable concentration are placed on aluminium discs or small plastic trays ( Figure 7.3) and applied to the back of the patient ( Figure 7.4), and then securely attached with hypoallergenic tape. These are removed and read at 48 hours, and then read again at 96 hours after application. A positive test results in an eczematous reaction at the site of application ( Figure 7.5).
Table 7.1 Uses of Wood’s light in vulval disease.
| Disease | Fluorescence colour |
|---|---|
| Vitiligo | Bright white |
| Infections | |
| Pseudomonas | Green |
| Erythrasma | Coral‐red |
| Tinea capitis – Microsporum species | Bright green |
| Tinea capitis – Trichophyton schoenleinii (Note: Other trichophyton species do not fluoresce) | Blue |
| Pityriasis versicolor | Copper‐orange |

Figure 7.3 Allergens for testing placed in plastic trays.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Ridley's The Vulva»
Представляем Вашему вниманию похожие книги на «Ridley's The Vulva» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Ridley's The Vulva» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.