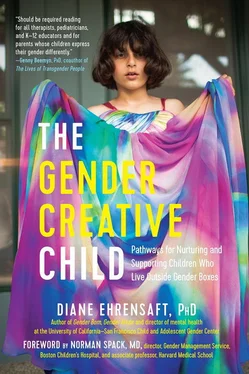
Diane Ehrensaft, PhD
THE GENDER CREATIVE CHILD
PATHWAYS FOR NURTURING AND SUPPORTING CHILDREN WHO LIVE OUTSIDE GENDER BOXES
To my beloved parents, Edith Ehrensaft and Morris Ehrensaft, ninety-six and ninety-eight years old, and still going strong
Foreword
by Norman Spack, MD
In 1985, WHEN I ran an adolescent medicine practice, a colleague asked me to provide testosterone treatment for a recent college graduate, my first transgender patient. Although the patient had been born anatomically female and had reached full female puberty, he went through college as a male with the support of his three male non-trans roommates, who kept his secret.
Treatment was simplistic and insufficient then, especially for patients transitioning from male to female. We only treated adolescents over the age of sixteen (post-puberty) who had been referred by highly experienced therapists, of whom there were few who worked closely with gender-nonconforming young people. No psychological tests were performed, no blockers given to suppress the hormones from the ovaries or testes.
The cross-sex hormonal protocols used for those patients transitioning from female to male were identical to those used for genetic males born without testes or with low levels of testosterone. Even patients who had undergone full puberty could cease menstruating with normal male replacement doses of testosterone. The patients emerged much the way they do now: bearded, with a male build, although often short for a male, and in need of mastectomy to flatten the chest. They looked so virilized that, when clothed, only someone with knowledge of their history would guess their anatomic birth sex.
In contrast, it took massive doses of estrogen to feminize anatomic males. It remained difficult to suppress undesired erections. And it was nearly impossible to adequately suppress the testosterone levels in patients with functional gonads. Thus, breast development was usually suboptimal, causing many patients to bear the added expense of augmentation surgery. In sum, at the time, I felt that the available treatment for my patients, even those who arrived as young as sixteen, was inadequate. If born anatomically male, they had difficulty passing for female in society, which contributed to their depression. If born anatomically female, they arrived too late to have prevented unwanted breast development and menses.
The approach to understanding gender-nonconforming children, too, was insufficient. Criticized for supporting their children’s transgender identity, parents were told by some prominent therapists to restrict access to toys and clothes of the opposite sex. Fortunately, that seemingly punitive attempt to redirect children from becoming transgender has been discredited. In her seminal book, Gender Born, Gender Made (2011), Dr. Diane Ehrensaft describes the more compassionate way for parents to support their children.
Approaches to early pubertal adolescents have also taken a sharp turn. In 1998, pediatric psychologists, psychiatrists, and endocrinologists at the Free University Medical Center in Amsterdam initiated treatment with reversible blocking drugs to suppress pubertal hormones at the inception of puberty. Their protocol was based on the hypothesis that, while prepubertal children of both sexes are similar in appearance, pubertal hormones cause permanent physical changes that interfere with the physical form they desire. In a state of pubertal arrest, patients gain time to be further evaluated, to come to terms with their gender identity, and to understand the medical consequences of taking irreversible hormones of the opposite sex, including infertility. Once patients reach the age of fifteen to sixteen, the Dutch add testosterone or estrogen treatment to the blockers in normative doses . In our clinic, virilizing breast removals are done at ages fourteen to sixteen, and feminizing genital surgeries are delayed until ages seventeen to eighteen.
In 2007, with the blessing of the chief of the endocrine division and the most senior administrative leadership at Boston Children’s Hospital, I cofounded the Gender Management Service (GeMs), following the Amsterdam model. The research conducted in Amsterdam, published in 2014, has shown the efficacy, safety, and psychosocial well-being that results from this approach. The GeMs was the first pediatric academic center in North America to open a medical clinic for transgender adolescents. In 2008, Dr. Diane Ehrensaft cofounded the Child and Adolescent Gender Center at the University of California, San Francisco. They, too, treat children and teens with hormone blockers. And, most importantly, Dr. Ehrensaft and others like her promote the gender affirmative approach—an effort to aid children in affirming their authentic gender rather than influencing them to accept the gender that would match the sex assigned to them at birth.
In 2009, the Endocrine Society, the largest and most prestigious international association of endocrinologists, released the Endocrine Treatment of Transsexual Persons , which recommended pubertal suppression as the treatment of choice in earliest puberty. The American Psychiatric Association’s fifth edition (2013) of the Diagnostic and Statistic Manual of Mental Disorders (DSM V) replaced its former term “gender identity disorder” with “gender dysphoria.” In an instant, transgenderism was no longer an inherent psychiatric disease. As a result of these groundbreaking publications, insurance companies could no longer justify denial of medications and surgeries. Pediatric endocrine and adolescent medicine divisions were empowered to create medical clinics for transgender youth. By 2015, fifty such programs had sprung up in North America, and the numbers continue to grow.
The evolution of counseling and medical treatment for adolescents has not been so straightforward, however. It has been like opening one of those wooden Russian dolls and finding another smaller one inside. In focusing on adolescents, we were reminded that we had missed the opportunity to provide ongoing support for the parents of children with gender dysphoria who felt isolated and confused by the conflicting opinions of academic clinicians. Dr. Ehrensaft’s guidance via her landmark interview on National Public Radio in 2008 and her book Gender Born, Gender Made was a balm for these families, who have literally been held together by this original work. Consistent with Dr. Ehrensaft’s teachings, our clinic is now staffed to offer intensive support for such families.
Then another Russian doll appeared. Patients arrived with issues that were new to us, although not to Dr. Ehrensaft. Referring to themselves as “genderqueer” or “gender fluid” (the term I prefer), these teens rejected any permanent gender identity. Their parents were understandably at wit’s end and in need of experienced advice. Fortunately, they can receive support in this newest book of Dr. Ehrensaft’s, The Gender Creative Child . Her recommendations will ease the journey for even more families with gender creative children. Dr. Ehrensaft’s wisdom is equally essential for and accessible to their therapists, physicians, evaluating psychologists, and teachers, as well as all of us who struggle to understand gender fluidity.
NORMAN SPACK, MD,is the director and cofounder of the Gender Management Service clinic at Boston Children’s Hospital, the first US clinic to medically treat transgender children. Dr. Spack has helped pioneer the use of hormone blockers to delay puberty and of hormone replacement therapy in teens. He has received national attention for his 2014 TEDx Talk “How I Help Transgender Teens Become Who They Want to Be” (over one million views) and was featured in Diane Sawyer’s landmark interview with Bruce (now Caitlyn) Jenner. Dr. Spack is associate professor of pediatrics at Harvard Medical School.
Читать дальше