To supplement the work of ILINet, Maryland also has a group of volunteer labs that send samples of flu strains they’ve collected to the state health department for testing on a regular basis. “This is a lab that’s just designed for surveillance,” Blythe said. “We can do the testing that tells us whether it’s AH3 or N1, and we can determine if it’s a pandemic strain.” And if they discover a new pandemic strain, they ship it to the CDC in Atlanta. Maryland is also working on a way for low-income and homeless people to report when they have the flu as well, since they tend to fall outside the health department’s surveillance network. “We know that many people with flu never seek out a health-care provider at all,” Blythe lamented. The Maryland Department of Health and Hygiene tries to remedy this by asking people to report in when they or somebody they know has the flu, even if they don’t go to the doctor. The agency also tracks illnesses in health-care workers, since they are often on the front lines when pandemic strikes. “If a new strain of SARS”—severe acute respiratory syndrome—“starts in Maryland and nobody recognizes it as SARS, the first place you’d see people getting sick would be hospitals, so we have surveillance to try to pick up that phenomenon,” Blythe explained.
Patterns of infection
Though a deadly pandemic could arise from the flu, it might also be a product of that ancient scourge the plague. A mutation in Y. pestis, the plague-causing bacteria, could leave us vulnerable to one of the deadliest diseases humanity has ever confronted. We might also find ourselves battling SARS, or (less likely) a virus like Ebola, which causes the extremely deadly and infectious viral hemorrhagic fever.
Regardless of the microbe that threatens us, a pandemic proceeds through eight recognizable stages, from incubation in animals at stage 1 to full pandemic in multiple countries at stage 6 (the peak of the pandemic). The next two stages, post-peak and post-pandemic, occur when the disease ebbs away until no one is infected anymore.
Nils Stenseth, a biologist with the University of Oslo’s Centre for Ecological and Evolutionary Synthesis, is an expert on plague. He and his colleagues lay out the typical scenario that most people expect for a pandemic, based on what they know of historic Black Death outbreaks:
In this classic urban-plague scenario, infected rats (transported, for example, by ships) arrive in a new city and transmit the infection to local house rats and their fleas, which then serve as sources of human infection. Occasionally, humans develop a pneumonic form of plague that is then directly transmitted from human to human through respiratory droplets.
Like the flu scenario in Contagion , this pandemic starts by infecting animals and quickly spreads to humans living in cities. Though Stenseth cautions that modern pandemics don’t always bloom first in cities, most pandemic modelers take cities as the fundamental points of contagion—the dots on a map that spawn red vectors of infection.
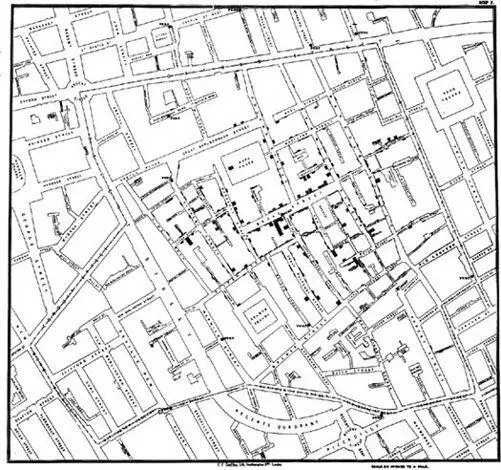
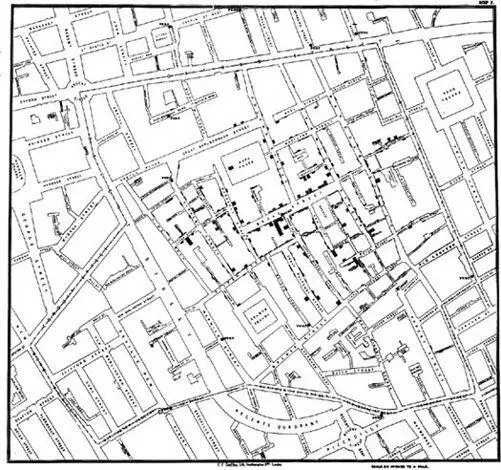
John Snow’s famous map of London, in which he tracked a cholera epidemic to its source in a well. You can see where he drew lines for numbers of dead in each location. He zeroed in on the well by tracking where the greatest numbers of deaths had occurred. (illustration credit ill.13)
But how do we predict where those red vectors will go once they’ve left the city behind? There’s one major difference between the Black Death hitting London in the 1340s and SARS hitting Hong Kong in 2003: air travel.
Though the SARS outbreak began in mainland China, investigators with the WHO and the CDC tracked its global spread to one isolated incident at Hong Kong’s Metropole Hotel. A medical professor visiting from southern China, where SARS had been claiming lives for a few months, checked into a small room on the ninth floor. Within days, 16 guests and visitors to that floor had also come down with the illness—many of them becoming sick after they’d flown to other cities all over the world, from North America to Vietnam. Investigators later came to call this incident a superspreading event, and traced it back to a hot zone on the carpet in front of that infected medical professor’s hotel-room door.
Even three months after the professor had checked out of the hotel, technicians were able to find SARS viruses in the carpet. In its report, the WHO speculated that the sick professor might have vomited outside the door to his room, leaving behind a massive number of live viruses that survived a cleanup from hotel staff. Somehow, those viruses wound up in the lungs of 16 other people who passed near the hotel hot zone, and carried it all over the world—starting what nearly became a pandemic.
Incidents like the one in the Metropole Hotel have led pandemic modelers to build air-travel routes into nearly all their outbreak scenarios. Tini Garske is a mathematician and researcher with the Imperial College London’s Centre for Outbreak Analysis and Modelling, and she’s spent most of her career modeling disease outbreaks. Her most recent work focuses on generating outbreak scenarios based on Chinese travel patterns. She and her colleagues surveyed a group of 10,000 Chinese people from two provinces, looking at typical travel patterns in both rural and urban regions. What they found was that pandemics emerging in rural areas are likely to spread “sufficiently slowly for containment to be feasible,” because most people surveyed rarely traveled outside their local areas. Economically developed urban areas make containment more difficult, owing to the numbers of people traveling great distances on a regular basis.
It would seem that the answer is simply to prevent people from traveling during a pandemic. But by the time we know we’re in the midst of a pandemic, it’s too late. Many other models show that limiting air travel makes almost no difference when it comes to limiting the spread of disease—at most, this tactic could delay the spread by a week or two. There are, however, a few superior methods based on models that take Garske’s travel research into account, and that incorporate what we learned during the SARS near-pandemic and the H1N1 (swine flu) pandemic of 2009.
Social distancing
Usually the first strategy that comes to mind for stopping pandemics is quarantine. In a typical quarantine, the government separates people who have been exposed to the disease from the general population. Ideally, people who have the pandemic disease are isolated both from the general population and from the quarantined.
During the SARS outbreak in Toronto, the Canadian government quarantined hundreds of people, and a number of large public events in the city were canceled, in an effort to contain the disease. After the dust settled, however, many medical experts, including representatives of the CDC, argued that the local government had overreacted, quarantining roughly 100 people for every SARS case. The chief of staff at York Central Hospital in Toronto, Richard Schabas, criticized the city sharply in a letter to a Canadian journal devoted to infectious disease: “SARS quarantine in Toronto was both inefficient and ineffective. It was massive in scale,” he wrote. “An analysis of the efficiency of quarantine in the Beijing outbreak conducted by the American Centers for Disease Control and Prevention concluded that quarantine could have been reduced by two-thirds (four people per SARS case), without compromising effectiveness.” In other words, the mass quarantines we see in virus horror movies like I Am Legend are not the way to stop a pandemic. They burn through health-care resources and are ineffective.
Читать дальше




![Аннали Ньюиц - Автономность [litres]](/books/424681/annali-nyuic-avtonomnost-litres-thumb.webp)