Jennifer Worth - In the Midst of Life
Здесь есть возможность читать онлайн «Jennifer Worth - In the Midst of Life» весь текст электронной книги совершенно бесплатно (целиком полную версию без сокращений). В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: Биографии и Мемуары, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:In the Midst of Life
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:3 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 60
- 1
- 2
- 3
- 4
- 5
In the Midst of Life: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «In the Midst of Life»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
In the Midst of Life — читать онлайн бесплатно полную книгу (весь текст) целиком
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «In the Midst of Life», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
These DNAR documents have no expiry date and, once signed, are valid until the patient dies or the order is changed for whatever reason.
DNAR in most cases would refer to CPR only, but also has the flexibility to allow withholding other treatment such as artificial nutrition and hydration – although these treatments tend to apply to patients already in hospital. Other ambulance services are working around the Allow a Natural Death (AND) procedure.
What is encouraging, of course, is that the ambulance service is now very much part of the integrated multi-disciplined team, and is consulted by the various primary care trusts in end-of-life care issues; and our concerns and wishes are being registered and used, helping us all with the treatment and services we can offer to patients as they reach the end of their natural lives.
Advancement in training, education, and the ever-increasing policies and protocols we follow now, will no doubt lead to an older, and healthier, nation. It is an amazing fact that treatments that we currently use already lead to heart attack and stroke patients recovering fully and going back to ‘tax paying’ status in a few short weeks. Twenty years ago, these patients would have died, or become paralysed for the rest of their lives.
I often chat with my work colleagues and ask them the searching question, ‘Have you thought about how and where you would prefer to die?’
I am surprised that most of them haven’t even thought about their own death, or what their personal preference is. This alarms me, considering the amount of death we actually deal with in our line of work!
For my own part, should I be suffering from an incurable illness, I will be instructing my GP and get my own DNAR written out, and I will leave it in a big white envelope just by the front door - in the hope that the young, keen ambulance crew who come rushing in will take note, and leave me to die in the peace I hopefully have earned!
APPENDIX III
Should patients at the end of life be given the option of receiving CPR?
by Madeline Bass, BSc, RGN, Head of Education, St Nicholas Hospice, Bury St Edmunds, Suffolk
First published in Nursing Times; 105 4, 26-02-2009.
Cardio-pulmonary resuscitation (CPR) is often unsuccessful and may not always be appropriate at the end of life. This article debates whether the use of cardio-pulmonary resuscitation by healthcare professionals in situations when it is unlikely to be successful feeds an unhealthy appetite to intervene just because it is possible. It explores the problem of offering patients and relatives the choice about CPR at the end of life when it is likely to be unsuccessful.
End-of-life and palliative care has become an increasingly important area of healthcare professionals’ work following publication of the End of Life Care Strategy (Department of Health, 2008).
Good communication between patients and staff is essential for those who are making choices and decisions about care at the end of life. This may include discussions about cardio-pulmonary resuscitation.
We can now treat disease and disability in ways that would not have been thought possible sixty years ago. These achievements have also created bioethical dilemmas. The advent of new treatment interventions has brought its own unhealthy appetite - the more treatments healthcare workers have to offer, the more they intervene. To them, this equates with doing the best for patients and knowing that everything has been tried.
However, in some cases, interventions can mean poor outcomes for the patient and result in low staff morale. One area of particular concern is the decision about when it is appropriate to perform CPR.
The media’s interpretation of CPR, primarily through TV drama, has led to a misunderstanding that it is a quick intervention that guarantees success without any side-effects (Bass, 2003; Diem et al, 1996).
CPR was first used in its present advanced life-support format of chest compressions, ventilation and defibrillation in i960 (Kouwenhoven et al, 1960). The main problem associated with CPR is identifying when it is appropriate to instigate it as a life-saving measure. The concern is that the decision to proceed is often viewed as the default if a decision about resuscitation has not been made.
CPR was devised as an emergency intervention for unexpected cardiac or respiratory arrest (Kouwenhoven et al, i960) and the majority of healthcare professionals are not aware that the success rates for CPR are very low (Wagg et al, 1995; Miller et al, 1993) (see Table 1). Only a small percentage of people will survive to leave hospital following a cardiac or respiratory arrest.
Ewer et al (2001) looked at the success rates of CPR undertaken on patients with cancer. They asked whether patients were expected to have an irreversible cardiac or respiratory arrest. The results showed that, of patients having an unexpected, reversible arrest, there was a 22.2% success rate. However, for those who were expected to have an irreversible arrest and were at the end of life, there was 0% success.
The effects of inappropriate CPR are often not considered. These include post-resuscitation disease (complications caused by resuscitation itself) (Negovsky and Gurvitch, 1995), an undignified death for the patient, and distress to relatives. Paramedics and resuscitation teams may also become demoralised by repeated failures (Jevon, 1999).
Table1 . Success rates for CPR
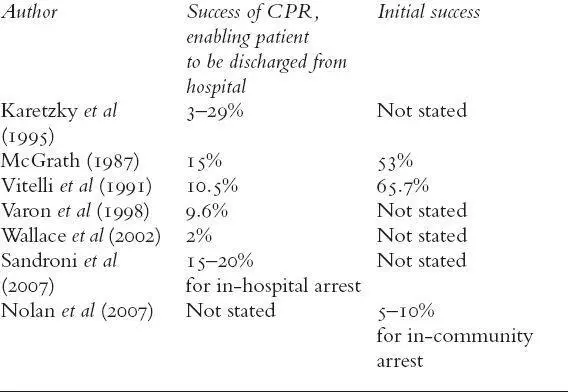
The success of CPR is often measured in terms of initial success - the return of heartbeat and breathing, controlled independently by the patient. It is also measured in terms of survival to discharge (see Table 1). The chances of successful CPR are improved if
There is early access to a cardiac arrest team
Basic life support is commenced immediately
Defibrillation is carried out as quickly as possible in cases of ventricular tachycardia or pulseless ventricular fibrillation (Jevon, 2002).
Other positive factors associated with a successful CPR attempt include:
A non-cancer diagnosis
Cancer without metastases
The patient is not housebound
Good renal function
No known infection
Blood pressure within normal range
The patient has robust health (Newman, 2002).
The Gold Standard Framework (GSF) suggests that cancer, organ failure, general frailty and dementia are not associated with success (NHS End of Life Programme, 2007).
The BMA et al (2007) recommended that CPR should not be attempted when patients have indicated before the cardiac arrest that they would refuse it or if the attempt is likely to be futile because of their medical condition.
Discussions about resuscitation at the end of life raise a number of questions.
Are public expectations of healthcare and technology unrealistic?
Do healthcare professionals pursue the possibility of an immediate positive outcome from CPR without considering the long-term consequences of the intervention?
Does inappropriate CPR raise false hope in patients, relatives and staff? (Jevon, 1999)
Awareness and knowledge of CPR guidance among healthcare professionals is poor (Bass, 2003), with knowledge focusing on local policy rather than research evidence and national guidance.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «In the Midst of Life»
Представляем Вашему вниманию похожие книги на «In the Midst of Life» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «In the Midst of Life» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.