General symptoms of low blood sugar – the two stages
STAGE ONE SYMPTOMS – FALLING BLOOD SUGAR
The immediate symptoms that follow a fall in blood sugar result from a reduction in the brain and nervous system fuel (i.e. glucose). These first stage symptoms generally include mental and physical lethargy, partial or total loss of concentration, headaches, trembling and/or dizziness, a tendency to yawn, paleness of lips and face with either a skin coldness or heat with perspiration, unexplained anxiety and a sudden urge for chocolate or anything sweet.
STAGE TWO SYMPTOMS – ADRENAL COMPENSATION
The second stage symptoms are caused by the adrenal response to the low blood sugar level. For many people these symptoms are more distressing than those of the first stage.
The surge of adrenaline that occurs in response to low blood sugar causes symptoms identical to the body’s response to stress. The metabolism is literally revved up for action. The heart rate increases and the blood flow to muscles is stepped up. This can be likened to pulling out the choke on a car to increase the available fuel. Heavy sweating can occur, with breathlessness and unpleasant palpitations.
A frequent consequence of the stress reaction is a degree of irritability or even aggression – a good example being the mood swings of the diabetic patient. Those readers who have a diabetic friend or relative will know only too well that when a ‘hypo’ occurs the victim becomes both irritable and aggressive. Many people with low blood sugar symptoms show a degree of anxiety, irritability or depression – symptoms that often improve as their problem is resolved.
All this is part of our body’s normal reaction to stress. If we are confronted by an angry bull as we cross a field we need to increase our oxygenation, heart rate and muscle strength to hastily flee. Most athletes and competitive sports people know the value of this adrenaline effect, for the power and speed increase it can provide. They learn to control and at times to override the adrenal response to further their sporting goals.
For most of us this alarm-response by our body is in direct proportion to the intensity of the threat or stress. However, many who suffer with chronic low blood sugar lose their fine control and an adrenal hair-trigger response to stress of any kind leads to frequent and often unnecessary alarm-responses. When adrenaline is released on a regular basis for trivial reasons, many distressing symptoms can develop. Some sufferers, for instance, are frequently awakened at 3–4am bathed in sweat, anxious, with a rapid pulse and short of breath. This occurs because the adrenal response to their nocturnal low blood sugar is being inappropriately triggered and their metabolism is stressed.
Unfortunately, even when we sleep changes in the blood sugar can activate the adrenal response. Professor Hans Selye, who wrote the definitive first description of our response to stress in his landmark 1956 book The Stress of Life , described sleep as follows: ‘No one is ever absolutely at rest, while alive. Even during sleep, your heart, your respiratory muscles, your brain continue to work. It makes no difference that you are not conscious of this and that these activities require no voluntary effort on your part’.
Our management of stress is a very individual quality that depends on many factors. The amount and type of activity appropriate to a five-year-old child would be very stressful for a 75-year-old man and vice versa. Our stress load and our stress handling are unique to each of us. Stress can, of course, be on many levels, psychological, chemical, structural or environmental. It does not always need to be unpleasant or unexpected to give rise to symptoms. Enjoyable, planned events can also be stressful – excited children becoming sick at parties and sports people suffering asthma attacks are examples of this.
The most common triggers that can cause low blood sugar symptoms include one or more of the following:
Excessive sugar consumption.
 Unexpected shock from any cause.
Unexpected shock from any cause.
Unaccustomed or excessive exercise.
 A delayed or missed meal.
A delayed or missed meal.
 Excessive caffeine intake (e.g. cola drinks or coffee).
Excessive caffeine intake (e.g. cola drinks or coffee).
 Excessive alcohol.
Excessive alcohol.
 The 3- to 5-day pre-menstrual time for women.
The 3- to 5-day pre-menstrual time for women.
CHAPTER 4 The diagnosis of low blood sugar
I have diagnosed and treated patients with low blood sugar for 35 years, and over this time I have learnt that a simple diagnosis of ‘low blood sugar’ is rarely helpful for the patient and not always accurate. Indeed the diagnostic challenge with low blood sugar symptoms is to provide satisfactory answers to the following questions:
1Are the symptoms of low blood sugar seen in a patient the result of poor stress handling or a faulty diet, and therefore transient and probably reversible? or
2Are the symptoms the result of a chronic glandular imbalance, long-term stress, excessive reliance on caffeine, tobacco, alcohol and other drugs, or the many other factors associated with dysglycaemia?
In fact, many people with the symptoms of low blood sugar have several causes running parallel. As low blood sugar masquerades as so many different conditions, and can create such a diversity of symptoms, diagnosis can be difficult. For this reason, and others that will be discussed later, it is not wise to diagnose low blood sugar without professional help. Low blood sugar mimics very many serious diseases and it is therefore essential that the possibility of more serious causes for the symptoms is ruled out.
The clinical diagnosis of low blood sugar falls naturally into several stages.
Low blood sugar disorders can pass from generation to generation. It therefore follows that a detailed evaluation of a person’s family health is of considerable diagnostic value.
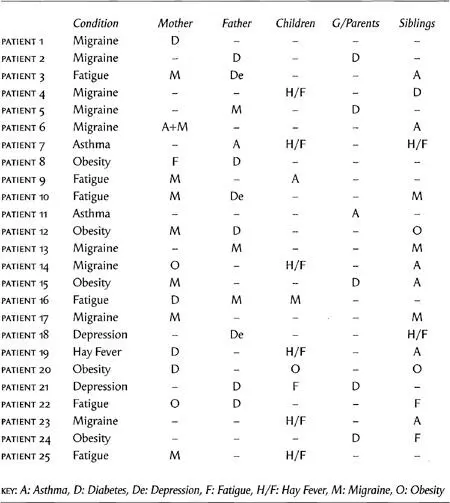
Table 1 – The family connection, 25 patients
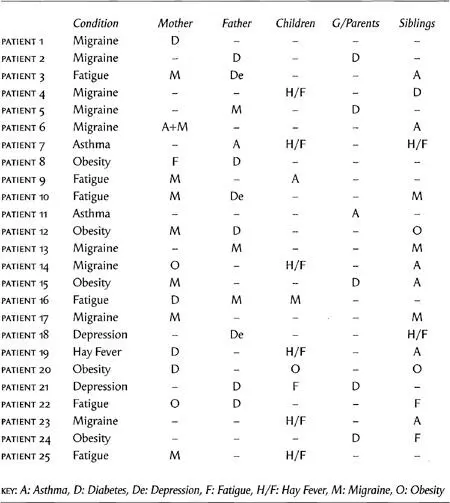
Table 1 illustrates the family history of 25 patients with confirmed low blood sugar. These patients have been selected because they are typical low blood sugar cases. You will see that characteristic disorders pass through each family. The majority of patients with low blood sugar symptoms tend to show a previous history in their family of either asthma, migraine, hay fever, diabetes, obesity, chronic fatigue or depression.
As we know, the symptoms of low blood sugar can be misleading to the diagnostician. Often of more significance than a list of symptoms are the pattern of cause and the time of onset of symptoms. One patient, Mr A, may experience headaches when reading or watching television, while another patient, Mr B, may develop headaches only in the early morning or when he drinks certain types of wine. In the case of Mr A, he may well have eyestrain, but Mr B could be suffering from low blood sugar.
Читать дальше
 Unexpected shock from any cause.
Unexpected shock from any cause.