Various studies suggest methods and materials to enhance the strength of the polymer formed by the adhesive system. Studies indicate that the use of a hydrophobic coating after the application of a simplified self-etch adhesive and an etch-and-rinse adhesive system provides a thicker and more uniform adhesive layer with lower concentrations of water and solvent and thus a significant reduction in fluid flow rate.235 ,240 This procedure transforms a simple-layer adhesive into a multilayer adhesive. This method ensures that the hydrophilic layer is photoactivated prior to the application of the hydrophobic, non-solvated bonding resin. This allows for the simplified adhesive layer to be more concentrated with hydrophobic monomers from the additional coating.212 ,232 ,241 Thus, by reducing the concentration of unreacted monomers between the primed and bonded layers, a more compacted and stable resin-dentin interface can be achieved.212 ,235 However, this modified protocol should be applied with caution to prevent a thick adhesive layer that could interfere with post seating.212 Numerous studies suggest that the application of ethanol to replace water in acid-etched collagen will allow hydrophobic resins to infiltrate the demineralized dentin and create a hydrophobic hybrid layer.231 ,239 ,242 ,252 Because endogenous matrix metalloproteinases (MMPs) become inactive in the absence of water, one study suggests that the application of ethanol is a potential mechanism for increasing the longevity212 ,250 and durability274 –276 of resin-dentin bonds. However, several authors indicate that ethanol wet bonding yielded higher immediate bond strengths and resulted in lower nanoleakage in root canals.237 ,246 Although there are differences in the suggested protocol in regard to concentration and time of application, a recent study suggested a simple higher concentration (50%) of ethanol for 60 seconds.266 Others indicate that using a high-intensity light-curing unit and/or increasing the irradiation time for the adhesive systems and resin cements will improve the adhesion of these systems to the canal wall dentin.228 ,230 ,244 ,249 One paper indicated that increasing the light-curing time improved bond strengths to root dentin.229
A myriad of studies suggests methods and materials for increasing the longevity of hybridization by improving the resistance of collagen fibrils to enzymatic degradation.207 ,277 ,278 Several studies suggest the application of chlorhexidine (CHX) as a protease inhibitor for MMPs261 and cysteine cathepsins270 to preserve the hybrid layer from degradation. Furthermore, several studies indicate that a 2% CHX or a CHX-containing phosphoric acid for etch-and-rinse adhesive systems may be an excellent method for increasing the long-term stability of collagen fibrils in the hybrid layer by inhibiting endogenous MMPs and cathepsins.268 ,269
It has been demonstrated that the use of ethylenediaminetetraacetic acid (EDTA) inhibits MMP-2 and MMP-9 when applied for 1 to 5 minutes,260 ,272 while one in vitro study indicated an application of EDTA preserved the dentin-adhesive interface.266 Thus, the use of EDTA has been indicated as a dentin pretreatment for dentin adhesives.212 ,266 However, one study demonstrated that prolonged rinsing with water removes the EDTA and there may be no residual EDTA to inhibit the degradation by endogenous MMPs.260 Several studies indicate that an increase in the extent of cross-linking of the collagen fibrils prior to adhesive application may increase the potential for durability, while other studies indicate that cross-linkers enhance the mechanical properties of these substrates. Cross-linking agents have been purported to have anti-MMP properties,253 ,257 thus reducing enzymatic degradation.273 However, the application time for desirable therapeutic effect is not feasible,279 ,280 and modification into a simplified protocol using proanthocyanidins incorporated into etchants and adhesives is recommended.254 ,256 ,258 ,259 Several studies indicate the use of benzalkonium chloride (BAC) or BAC-containing acid or adhesives to inhibit the activity of the endogenous MMPs.264 ,271 Because the root canal anatomy can impose limitations to achieving a quality hybrid layer, modified clinical protocols may have positive implications for improving the quality of the adhesive interface and the long-term adhesion of fiber-reinforced post systems to dentin. This in turn can improve the structural integrity of the remaining radicular dentin and increase the retention and resistance to displacement 55 ,168 ,281 while dissipating and reducing functional stresses along the entire adhesive interface, thus providing maximum post retention and core stability.
Conservation of tooth structure
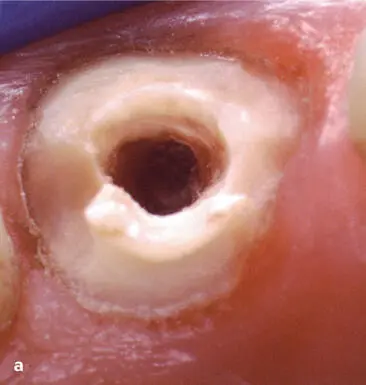
Numerous in vitro studies support evidence that conservation of sound tooth structure is the most important factor to the successful management of structurally compromised ETT. 47 , 51 ,216 ,282 –288 It is well supported in the literature that the longevity of an ETT is directly related to the amount of remaining sound tooth structure. 29 , 43 ,289 However, traditional-cast post systems and prefabricated post systems often require the removal of undercuts for a proper path of insertion and adaptation to the canal wall. This enlargement of the post-endodontic channel throughout biomechanical preparation during and after the endodontic procedure removes dentin during cleaning and shaping of the canal. The removal of additional dentin to accommodate placement of a larger post diameter significantly weakens the remaining tooth structure175 ,285 ,290 ( Fig 1-6). This widening of the canal decreases the thickness of the root wall, which can lead to a diminished wall stiffness that results in increased stress levels291 ,292 and can compromise long-term success.293 ,294 It is widely accepted that 1 mm of dentin wall thickness is required to prevent root fracture and to properly support the core.159 ,295
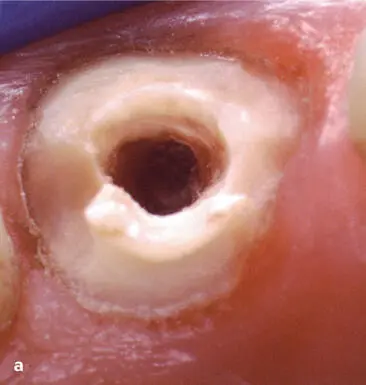


Fig 1-6 (a) Overpreparation of the post space to accommodate a larger selected fiber-reinforced post can weaken the remaining tooth structure and increase the potential for root fracture. (b) Root perforation caused by improper preparation and placement of an oversized post. (c) Repair of the perforation seen in b . (Dentistry in b and c courtesy of Riccardo Tonini, MD, DDS.)
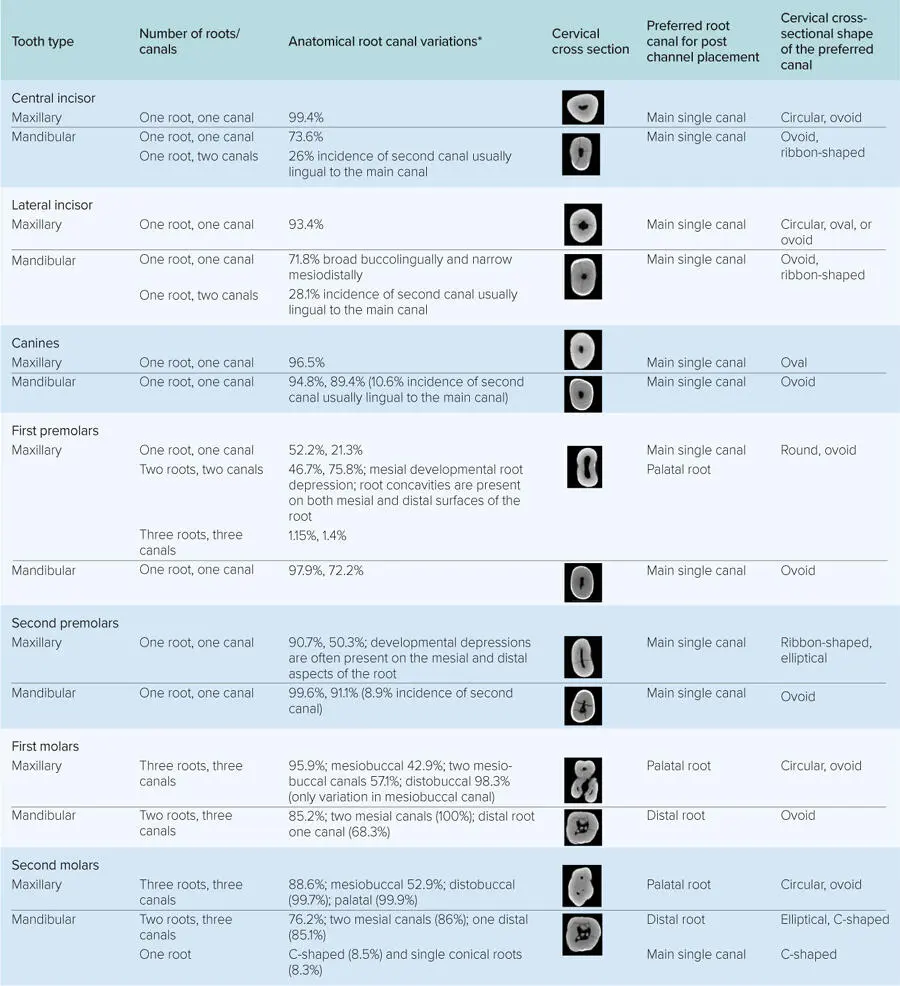
Table 1-1 General guidelines for post placement300 ,337 –339
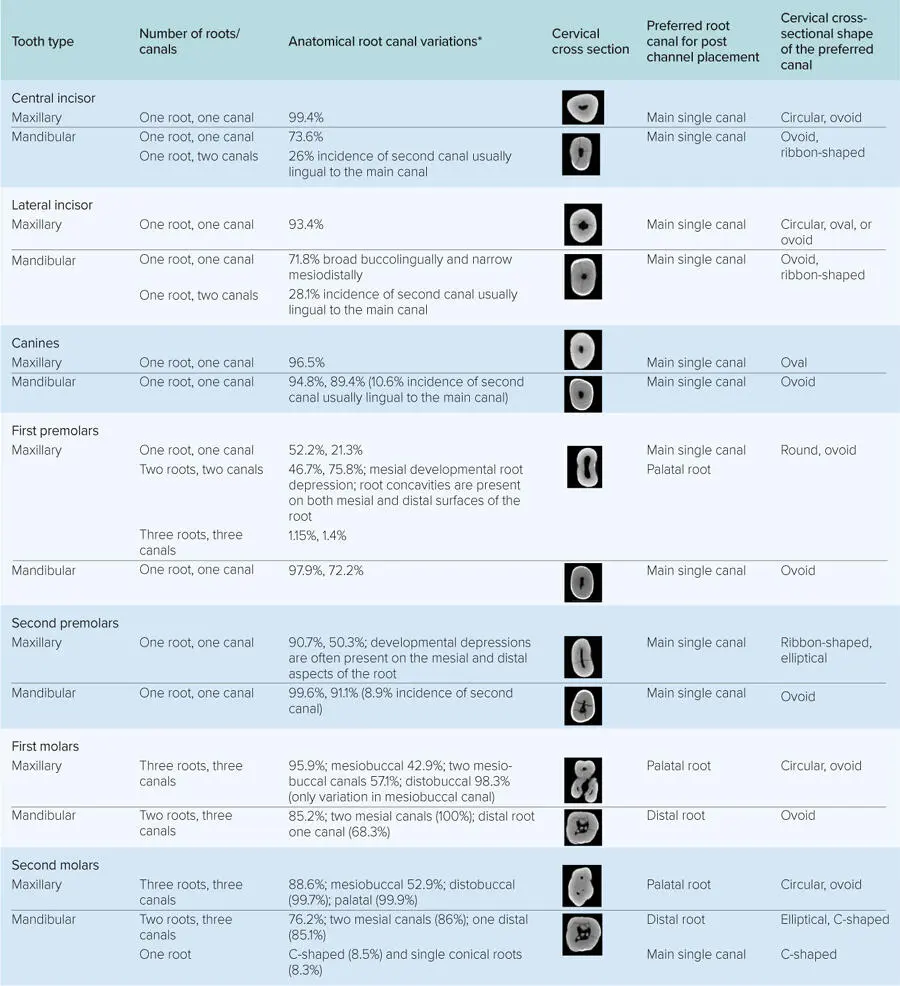
This table indicates anatomical root canal variations in Asian and non-Asian populations. However, anatomical variations exist in different subpopulation groups. The table provides the necessary information for post preparation and placement. During post channel preparation, the preservation of 4 to 5 mm of gutta-percha is necessary to provide an adequate apical seal.201 ,296 –307
*If there are two numbers, the first number is the prevalence for that number of roots for a given tooth, and the second number is the prevalence for that number of canals for said tooth among the population groups studied.
Additionally, during post channel preparation, the preservation of 4 to 5 mm of gutta-percha is necessary to provide an adequate apical seal.201 ,296 –307 Several techniques for preparing the post channel and the effect of each technique on the apical seal have been investigated and include the use of rotary instruments, heated instruments, and solvents.175 ,299 ,304 ,308 –310 An improper access preparation with too wide an enlargement when performing endodontic therapy can result in an excessive loss of sound coronal tooth structure 20 , 40 ,311 ,312 and increase the occurrence of fractures 43 ,206 ,291 ,313 ( Fig 1-7). In addition, endodontic access on a tooth with loss of one or both marginal ridges increases the potential for fracture. 29 , 44 ,314 –317 Investigators have reported that rotary instruments caused more dentinal defects, such as craze lines and partial cracks, which have the potential to develop into fractures after endodontic and restorative treatment.318 –320 However, no defects were observed with hand file instrumentation.318 Furthermore, overpreparation of the post space and the utilization of larger posts decrease the resistance to fracture. 51 ,285 ,287 This reduction in the amount of dentin weakens the structural integrity of the tooth216 and can be responsible for horizontal and vertical root fracture.291 ,321 –326 To prevent overpreparation during the endodontic or restorative procedure, it is recommended that the root morphology be considered for each tooth type prior to treatment. Mandibular incisors, maxillary second premolars, and the distal root of mandibular molars have mesiodistal concavities and may be narrower mesiodistally than they appear in the radiograph.327 A CBCT image can provide a 3D visualization of these anatomical features in cross section and reduce the potential for a weakened structural integrity or root perforations328 by providing a view of the tooth anatomy. Because of the wide range in anatomical variation in regard to number and shape of roots and root canals for each tooth type,329 –335 a comprehensive knowledge of root morphology179 ,336 and an understanding of external root anatomy can provide insight for selecting the teeth and roots that are most appropriate for post placement with less potential for thinning and root fracture300 ( Table 1-1; for further information, see section entitled “Guidelines for Restoring the Intraradicular Space”300 ,337 –339).
Читать дальше